In the complex, rapidly evolving landscape of healthcare, the prior authorization (PA) process emerges as a critical yet challenging checkpoint. This activity, essential for verifying coverage for treatments, medications, or equipment before they are provided to patients, stands at the heart of cost control and the delivery of appropriate care. Yet, its traditional management is wrangled with inefficiencies that cause delays, increase costs, and frustrate both providers and patients. In fact, 93% of healthcare providers report care delays while waiting for insurers to authorize necessary care with 82% highlighting that authorization can lead to treatment abandonment because of prior authorization struggles with their insurance company.
These inefficiencies are contribute to the estimated $950B spend on administrative functions and are a source of frustration for healthcare payers, providers and patients alike.
Recent advancements in technology, however, have stirred heightened interest around artificial intelligence (AI) within the PA process, with its potential to automate 50 -75% of manual tasks.
Let's look closer at how AI can transform the prior authorization process and what the transformation could look like for your organization.
The Current State of Prior Authorization
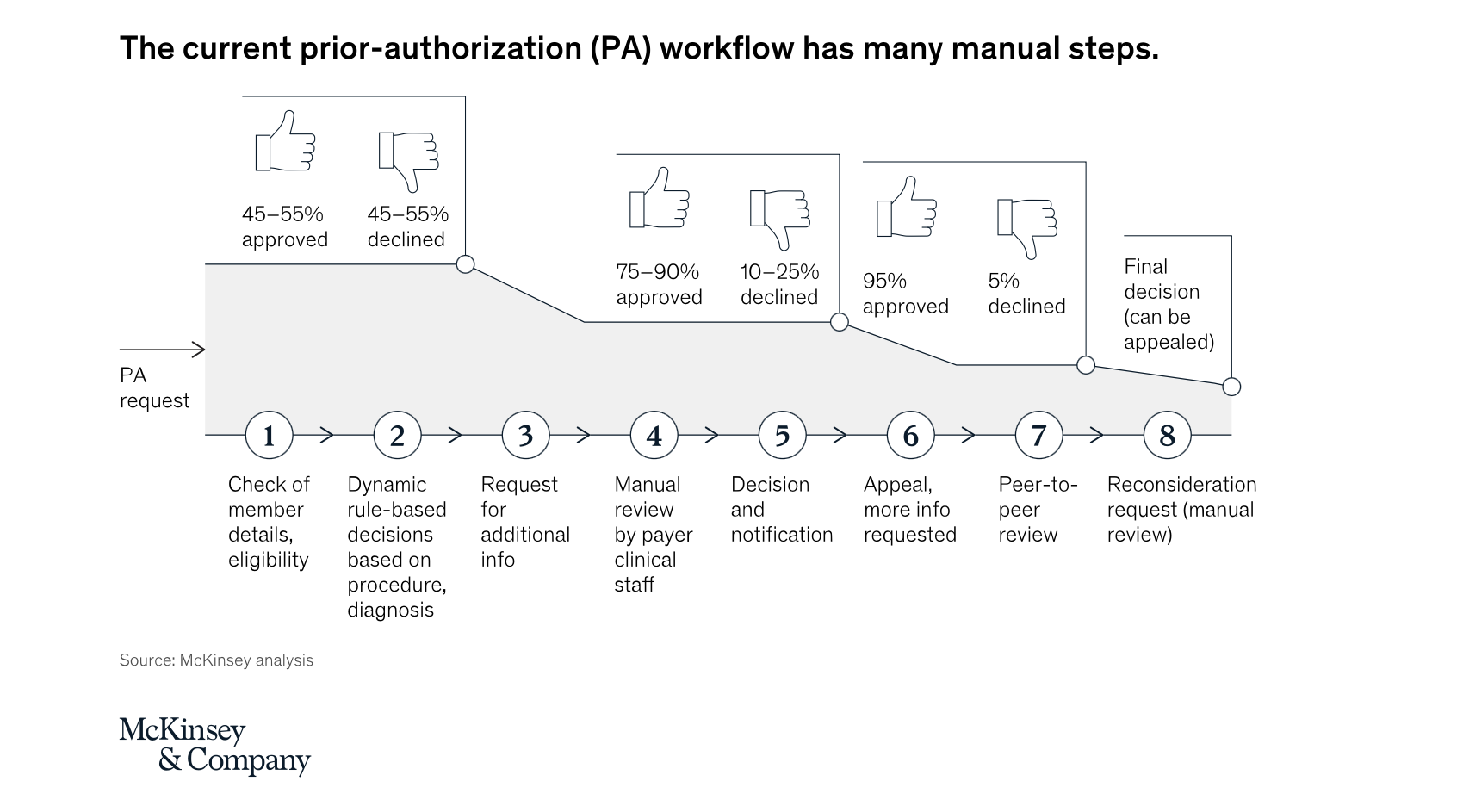
Today's prior authorization process is extremely labor-intensive and time-consuming, as evidenced below in a digram from McKinsey & Company. This process involves a lot of moving parts that affect providers, payers, and patients. While there are accepted guidelines on some issues, the lines are blurred on others. To get a better understanding and get answers to some of the most frequent questions, download The Ultimate Guide to Prior Authorization from our partner, Myndshft.
The statistics surrounding prior authorization underscore the urgency of the situation. According to a survey by the American Medical Association (AMA), more than 84% of physicians describe the burden of PA as high or extremely high, with each physician completing an average of 31 PAs per week. This not only leads to administrative overload but also can delay patient care. In some cases, these delays can have significant health implications, especially in time-sensitive situations. In some instances, these delays can have dire consequences, emphasizing the critical need for a streamlined and efficient process.
The Critical Challenges of Prior Authorization
The statistics surrounding prior authorization underscore the urgency of the situation. Over 84% of physicians report that the administrative burden of PA is high or extremely high, with each physician dealing with an average of 31 PA requests per week. This labor-intensive process, reliant on outdated technologies such as fax machines and phone calls, not only creates a significant workload for healthcare providers but also leads to delays in patient care. In some instances, these delays can have dire consequences, emphasizing the critical need for a streamlined and efficient process.
Unlocking Efficiency With AI
AI has the potential to significantly alleviate the burdens associated with PA. By automating routine tasks, enhancing decision-making with predictive analytics, and improving communication channels, AI can streamline the PA process in several ways:
-
Automating Routine Tasks: AI can automate the collection and processing of patient data required for PA. By integrating with Electronic Health Records (EHRs), AI algorithms can extract necessary information, fill out forms, and submit them to insurers automatically. This reduces manual errors and saves substantial time for healthcare providers.
-
Predictive Analytics: AI can analyze historical data to predict the likelihood of a PA request being approved. This helps healthcare providers make more informed decisions about whether to pursue a PA request or consider alternative treatments that do not require PA.
-
Natural Language Processing (NLP): AI-powered NLP can interpret and respond to written and spoken requests from healthcare providers. This technology can be used in chatbots or virtual assistants to help providers navigate the PA process more efficiently.
-
Enhanced Communication with Payers: AI can facilitate better communication between healthcare providers and insurance companies. Through AI-driven platforms, providers can track the status of PA requests in real-time, receive notifications about missing information, and get quicker responses from payers.
Challenges and Considerations
While AI offers promising solutions, there are challenges to consider:
-
Data Privacy and Security: Handling sensitive patient data requires strict adherence to privacy laws and regulations, such as HIPAA in the United States. Ensuring the security and confidentiality of data within AI systems is paramount.
-
Integration with Existing Systems: Integrating AI solutions with current healthcare IT infrastructure, such as EHRs, can be complex and require significant resources.
-
Provider and Patient Acceptance: Encouraging healthcare providers and patients to trust and adopt AI-driven processes is crucial. This involves education and training on how these systems work and their benefits.
-
Regulatory Compliance: AI systems used in healthcare must comply with various regulatory standards. Ensuring these systems are up to date with changing regulations is vital.
Lead the Way in AI-Powered Prior Authorization With NexAuth
Traditional prior authorization processes, known for their time-consuming and complex nature, often delay patient care and impose heavy administrative burdens on healthcare providers and payers. NexAuth, developed in collaboration with Google and Myndshft by Productive Edge, offers a compelling solution.
"At Google Cloud, we are committed to harnessing the power of technology to transform healthcare. Our collaboration with Productive Edge on NexAuth demonstrates how leveraging cutting-edge AI and machine learning on processes like prior authorization reduces administrative burden, time to care, and cost. NexAuth can streamline existing workflows relatively quickly in a secure, scalable environment. The benefits add value to payers, providers, and, most importantly, patients waiting for care." - Amy Waldron, Director, Healthcare & Life Sciences Strategy & Solutions
By harnessing the power of AI-enabled capabilities, NexAuth equips healthcare payers to modernize PA processes, ensuring patients receive the timely care they need without the red tape. This AI-driven approach is not merely about boosting operational efficiency; it represents a critical move towards a more patient-centered healthcare system, marking a significant stride in the evolution of healthcare delivery.
A Closer Look at NexAuth
Modular, AI-Enabled Services
NexAuth's strength lies in its modular design, offering flexibility to healthcare payers to adopt one or all of its services based on their specific needs. These services include:
-
Intake: Leveraging Google Cloud’s Document AI and Vertex AI services, NexAuth’s Intake feature streamlines PA submissions through AI-enabled document processing and validation, promising to cut manual attachment processing costs by 50%.
-
Case Validation: Utilizes smart software to verify patient details against a database of over 2,000 insurers, ensuring accurate and up-to-date insurance coverage for each case. This AI-assisted technology harmonizes compliance and can potentially decrease regulatory-related denials by up to 25%.
-
Clinical Recommendation and Clinician Review: These services harness Vertex AI to analyze submission data, policy coverage, evidence-based data, medical history, and guidelines. They provide personalized approve/deny recommendations and assist clinicians in reviewing PA requests more efficiently, summarizing information and responding to queries to accelerate decision-making.
By integrating these services seamlessly with existing PA workflows, NexAuth offers immediate value and aligns with long-term strategic objectives. The benefits are manifold:
- Automated Decision-Making: Accelerates the PA process, drastically reducing operational costs and decision times by up to 30%-50%.
- Reduced Administrative Burden: By automating routine tasks, NexAuth minimizes manual work, enhancing efficiency and enabling healthcare payers to do more with less. This automation is capable of reducing manual workload by 30%-50%, directly impacting the bottom line.
- Enhanced Patient Care: The efficiency brought about by NexAuth leads to faster patient care and reduced system frustrations, culminating in a more efficient, patient-focused healthcare experience.
Healthcare payers leveraging NexAuth can expect to handle increased PA requests without adding staff, harmonizing compliance across processes, and significantly decreasing the time and costs associated with PA decisions. With NexAuth, the path towards a more efficient, patient-centered healthcare system is clearer and more attainable than ever.
The Future is Now
The push to modernize prior authorization is clear, and tools like NexAuth offer healthcare payers a way to lead this change, ensuring patients receive care swiftly, cutting through red tape. This shift towards AI-driven PA processes marks a crucial move towards patient-focused healthcare, streamlining service delivery and enhancing outcomes. NexAuth not only simplifies the PA process but also aligns with the evolving landscape of healthcare, where efficiency, accuracy, and patient satisfaction are paramount. By embracing AI, such as NexAuth, the healthcare industry can transform PA into a more effective, fraud-resistant, and patient-aligned procedure, heralding a new era of healthcare management that benefits all stakeholders.
To learn more about integrating AI into your prior authorization processes, get in touch with one of our experts today.