Artificial intelligence in healthcare is no longer a distant idea — it’s here, it’s being piloted, and it’s starting to show measurable results. At the same time, many healthcare leaders are still wrestling with where AI fits into their organizations and how to move from experimentation to impact.
To explore this, I sat down with Raheel Retiwalla, Chief Strategy Officer at Productive Edge, for a mid-year check-in on AI in healthcare. Raheel has been on the front lines with both payers and providers, and he’s built more than 50 AI accelerators that model how specific workflows can be improved. In our conversation, we talked about what healthcare leaders are focused on, how they’re approaching AI adoption, and what it takes to succeed.
The Mood in Healthcare Around AI
Everyone in healthcare is talking about AI. Every vendor claims to have AI embedded somewhere, and leaders are flooded with options. Raheel points out that beneath the noise, three themes consistently rise to the top:
-
ROI: Executives want proof that AI will deliver measurable business value. Time savings and productivity gains are important, but they need to be tied directly to financial and clinical outcomes.
-
Governance and Responsibility: Healthcare organizations can’t afford black-box systems. AI solutions must be auditable, observable, and aligned with compliance and ethical guidelines from day one.
-
Too Many Point Solutions: Innovation is happening at a rapid pace, but with it comes a flood of disconnected tools. Leaders are asking how to sift through these and create a unified AI strategy that fits their enterprise architecture.
As Raheel puts it, “Healthcare leaders aren’t just experimenting anymore. They want a roadmap — a framework to bring all this innovation together.”
The Four Roles of AI
To cut through the noise, Raheel uses a simple model to describe the four key functions AI can play in healthcare workflows:
-
Summarize and Aggregate: Help staff organize information so they can act on it faster.
-
Recommend: Go beyond presenting data to suggesting the next best step.
-
Nudge and Activate: Surface opportunities in real time and guide action.
-
Execute: Automate routine, repetitive tasks so humans can focus on higher-value work.
This model helps organizations think systematically about where AI belongs and how to prioritize use cases.
Payers vs. Providers: Different Priorities
Payers and providers are approaching AI from different angles.
-
Payers are focused on integration. They want to understand where AI fits across complex workflows like utilization management, care management, and claims. Accelerators help them visualize how AI can slot into existing systems and build toward an enterprise strategy.
-
Providers, by contrast, are operating in a crowded market of point solutions. Their EHR remains the central system of record and data hub, but leaders are constantly asking: “What gaps does my EHR have, and which solutions can fill them?” Increasingly, they’re also looking at how to bring EHR data and engagement data together in CRM to create a unified view of the patient.
Both sides want results, but their paths to adoption look different.
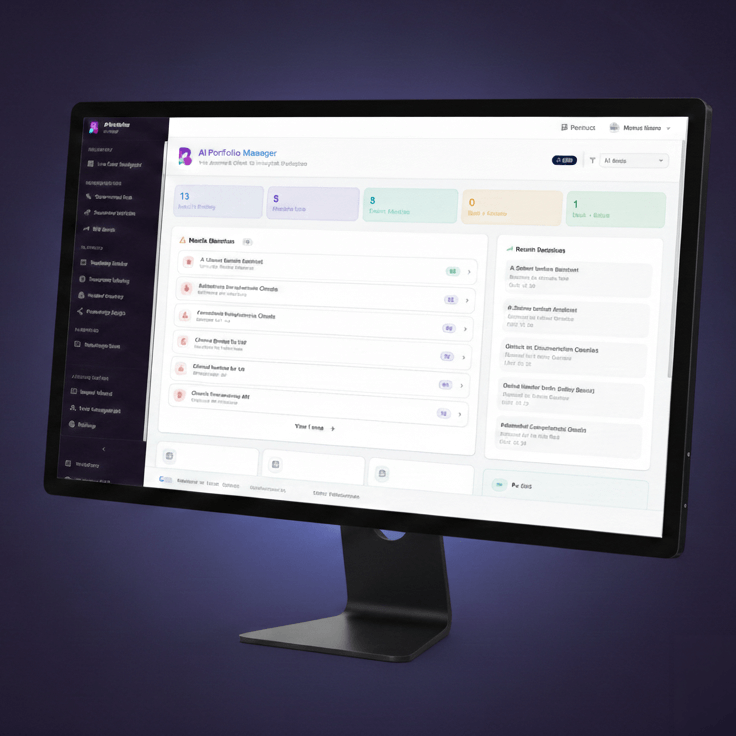
Accelerators in Action
To make these ideas real, Raheel and his team have developed more than 50 AI accelerators. These are practical, pre-built models of how AI can transform specific workflows. In the episode, Raheel shared a few examples:
-
Pre-Visit Face Sheet Generation: An accelerator that prepares care managers with a unified view of member history, medications, care gaps, and social determinants of health — cutting preparation time from nearly an hour to minutes.
-
Revenue Integrity Optimization: A provider-focused accelerator that surfaces missing or misaligned charges in near real time, reducing downstream denials and protecting margins.
Leaders value these accelerators because they’re not abstract. They’re concrete, visual, and easy to connect to day-to-day work.
How to Move Forward
So how should healthcare leaders move from exploration to execution? Raheel’s advice is clear:
-
Start with use cases: Identify workflows with high friction and measurable ROI.
-
Validate impact and feasibility: Balance business value with technical readiness.
-
Pilot quickly: Aim for results in 8–10 weeks, not multi-year projects.
-
Embed governance early: Treat responsible AI as a core design principle, not an afterthought.
With this approach, organizations can move beyond hype and start building an AI roadmap that delivers real value.
Listen to the Full Conversation
This is just a snapshot of our discussion. To hear the full conversation — including more examples of accelerators and practical advice for both payers and providers — check out the episode below.