AI is everywhere in healthcare headlines. New pilots, new tools, big promises. The momentum is real. But the real question isn’t how fast we can adopt AI. It’s whether we’re using it in ways that actually help—and help the right people, in the right places, at the right time.
A recent article highlighted how one large healthcare organization is rolling out AI. Their focus: cut administrative waste, support care decisions, and speed up research. All good goals. But their story points to something bigger.
Healthcare doesn’t just need more AI. It needs better thinking about how AI fits into the way care actually happens on the ground. Who is the AI for? What does it replace? What does it support? And how does it change the day-to-day work of real people delivering and receiving care?
Start with People, Not Tech
The best AI doesn’t show off. It works in the background. It handles routine tasks, pulls out key information, and frees people up to focus on care. That’s where the real impact is—in the minutes and mental energy saved.
Too often, AI gets layered on top of already broken processes. That just adds more work. You end up with more systems, more notifications, and more confusion. The point isn’t to impress with shiny new tools—it’s to make the work easier and the outcomes better.
Before adding AI, organizations need to ask: what’s already slowing people down? What’s fragmented, manual, or unclear? AI should be a fix, not a patch.
Don't Leave It to IT
Some organizations hand AI over to their innovation team or IT department and hope for the best. That’s a mistake. These teams are critical, but they can’t do it alone.
The smartest AI efforts bring together people from care, operations, compliance, and tech. It takes all of them to figure out where AI can actually help and how to roll it out without disrupting everything else.
This kind of cross-functional leadership isn’t easy, but it’s necessary. It builds alignment, speeds up decision-making, and ensures that AI efforts stay grounded in the reality of healthcare delivery.
Look for High-Value, High-Pain Workflows
Start where the friction is obvious and the impact is measurable. Prior authorization intake. Claims triage. Service plan creation. These are messy, repetitive, and time-consuming—and they matter to both cost and quality.
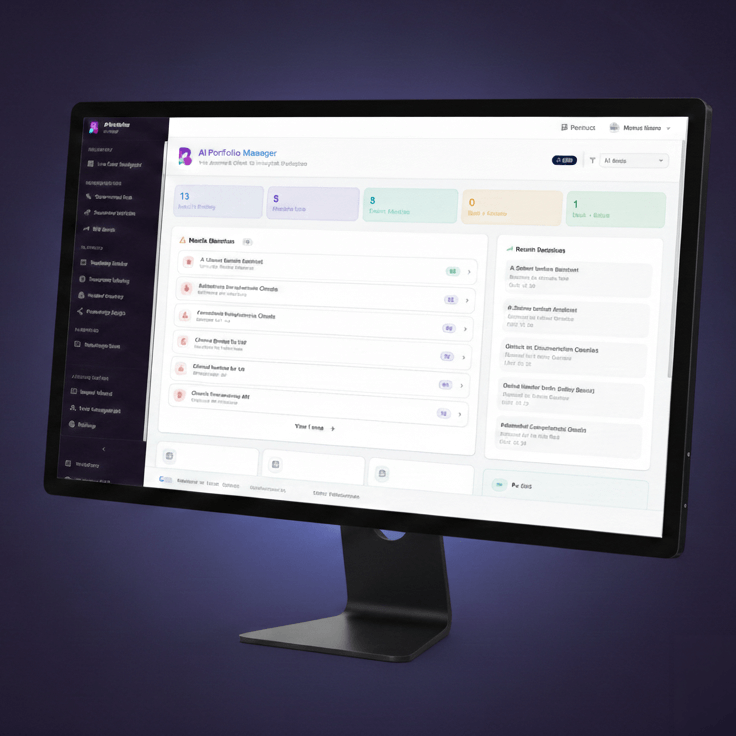
These areas are ideal for AI agents: modular, focused tools that observe, decide, and act based on structured and unstructured data. They don’t try to solve everything. They do one job well.
When used well, AI can help staff move through these workflows faster and more accurately. It won’t eliminate the work, but it can remove the drag—freeing people up to handle exceptions, escalate edge cases, or focus on care.
Build Trust from the Start
In healthcare, trust is everything. If people don’t understand what the AI is doing or how it’s making decisions, they won’t use it. Or worse, they’ll use it blindly and assume it’s always right.
That’s risky. Trust isn’t just about transparency—it’s about giving users enough context and control to feel confident.
So be clear about what the tools are doing. Give users ways to review, adjust, and provide feedback. Monitor performance and fix what’s not working. And above all, don’t roll out AI in the dark. Bring people into the process early and often.
Make Ethics Part of the Process
Bias, fairness, accountability—these aren’t side issues. They’re central to using AI safely and effectively. If the models aren’t designed and tested with care, they can do real harm. That includes reinforcing disparities, excluding vulnerable populations, or making care less personal.
Healthcare has always taken patient safety seriously. Ethical AI deserves the same level of rigor.
That means asking hard questions. Who trained the model? What data was used? What assumptions were built in? How do we monitor outcomes? And how do we fix problems when they show up?
Treating these questions as part of the normal workflow—not a separate track—will set up AI projects for long-term success.
The Bottom Line
AI has a role to play in fixing some of healthcare’s biggest problems. But it’s not a magic fix. It’s a tool—and it needs to be aimed at the right problems, with the right people leading the charge.
Start small. Focus on real pain points. Stay close to the people doing the work. Measure impact. Adjust as you go. And don’t lose sight of the human side.
That’s how we move from pilots and potential to results that last.