In the U.S. healthcare industry, administrative overhead is reaching a breaking point. Up to one-quarter of all healthcare spending is considered waste, largely due to administrative complexity. Both health insurers and provider organizations face intensifying pressure to do more with less, as costs climb and reimbursement rates lag behind. Workforce shortages and burnout compound the challenge, with frontline staff overwhelmed by paperwork and process inefficiencies. In response, many healthcare leaders are eyeing a new solution: AI agent technology to automate operational tasks and streamline workflows.
Healthcare organizations are turning to AI “agents” – effectively a digital workforce – to relieve administrative burdens. These intelligent agents can independently carry out routine workflows once given a goal and guardrails (Productive Edge). By automating mundane tasks, organizations reduce errors and staff burnout, allowing clinicians and employees to refocus on higher-value work and patient care. At the same time, these AI-driven solutions help control costs and boost efficiency, a crucial advantage when many cost pressures can only be addressed through automation.
The Pressure to Automate Administrative Tasks Now
Healthcare is notorious for its administrative bloat and manual processes. A 2019 study found that $760–$935 billion – roughly 25% of U.S. healthcare spending – is wasted, with administrative complexity the single largest contributor (JAMA). This isn’t just a financial drag; it also leads to burnout, workflow bottlenecks, and delays in care. Payers and providers alike are realizing that trimming this waste is essential to remain sustainable and improve service. In fact, for every $10 billion in a payer’s revenue, AI-driven solutions could save $150–$300 million in administrative costs (McKinsey). Industry analyses likewise estimate the system could save upwards of $20 billion by shifting common tasks (claims processing, eligibility checks, billing, etc.) to automated workflows (CAQH).
Beyond dollars and cents, there’s a human imperative to act. Burdensome admin tasks are sapping morale and contributing to a crisis in the healthcare workforce. Physicians themselves say the biggest opportunity for AI is reducing administrative workload – 57% of doctors in a recent AMA survey ranked that as AI’s top value (AMA Survey). In other words, the people delivering care are urgently seeking relief from paperwork. As staffing shortages grow, automating routine processes is no longer a “nice to have” – it has become critical to maintaining operations and patient satisfaction.
AI Agents: A Digital Workforce for Healthcare Operations
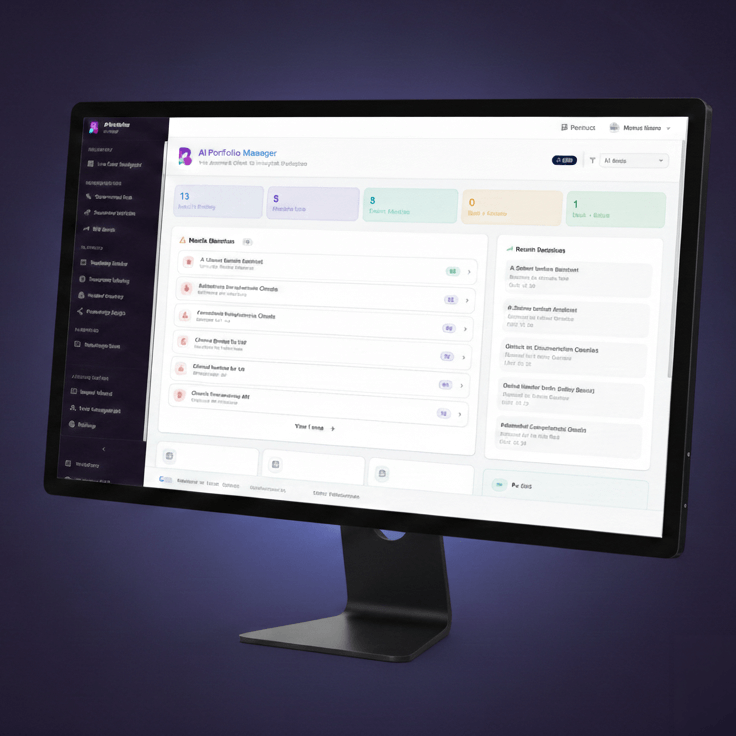
Enter AI agents: autonomous software assistants that can handle complex, multi-step workflows from start to finish. These aren’t just simple chatbots or scripts, but goal-driven virtual workers capable of reasoning, taking action across systems, and involving humans when needed (McKinsey). Think of an AI agent as a junior team member made of code – it can log into applications, cross-check information, send communications, and more, all under predefined guardrails. Crucially, agentic AI allows a spectrum of autonomy with a human-in-the-loop at critical points, so high-stakes decisions still get appropriate oversight.
Already, AI agents are being used to automate many administrative and operational tasks that bog down staff. Providers are using agents to coordinate patient access, identify sites of care, schedule appointments, and prepare patients. On the financial side, agents are streamlining revenue cycle workflows, including submitting claims, verifying codes and documentation, and drafting appeal letters for denied claims. Payers are deploying similar digital workers to handle member inquiries and prior authorizations, dramatically cutting turnaround times. Early implementations have already demonstrated measurable benefits, including faster processing and improved compliance (Productive Edge).
Payers vs. Providers: Build or Buy?
While both payers and providers feel the push to adopt AI agents, their approaches often differ. Health plans (payers) tend to lean toward building solutions in-house or via strategic tech partnerships. Many organizations have substantial IT and analytics teams and prefer custom AI development to tailor automation to their unique processes, while maintaining control over sensitive data (McKinsey).
Provider organizations, by contrast, typically buy vendor-built solutions. Outside of the very largest health systems, most providers have smaller IT departments and tighter budgets. Integration with existing systems (especially the EHR) is a top concern, which often leads them to adopt AI features from their incumbent vendors or plug-and-play solutions from trusted partners (Bain/BVP Healthcare AI Index). The bottom line: payers are more likely to build, providers are more likely to buy – but both paths require a clear strategy and disciplined execution.
Seizing the Opportunity
The case for AI agent-based solutions in healthcare operations is compelling – and the window to act is now. Organizations that move quickly will gain an edge in efficiency, cost-effectiveness, and workforce satisfaction. Those who delay risk falling behind as the industry transforms.
The good news is that you don’t have to navigate this shift alone. Productive Edge’s new eBook on AI agents for healthcare payers and providers lays out practical steps for deciding what to build, what to buy, and how to get started.
👉 Download the complete guide here to learn how your organization can reduce administrative burden and drive meaningful improvement.