NexAuth
An AI-Powered Solution for Prior Authorization

INTRODUCING NEXAUTH
Streamline Prior Authorization and Cut Costs with AI
Prior authorization is essential but can be a bottleneck in healthcare delivery, delaying treatment and increasing administrative burdens. Care Advisor: NexAuth is designed to change that. By applying advanced AI and machine learning to existing workflows, NexAuth accelerates decision-making, improves accuracy, and enhances patient and provider experiences.
Revolutionize Your Prior Authorization Process
With Care Advisor: NexAuth, healthcare payers can:
- Reduce Decision Times by Up to 40%: AI automates routine processes, significantly cutting down on manual paperwork and enabling faster approvals.
- Improve Accuracy and Compliance: AI-powered insights help your team make more precise decisions, reducing unnecessary denials and rework.
- Lower Operational Costs: By streamlining workflows, NexAuth can reduce administrative expenses by up to 30%, allowing payers to reinvest savings into patient care and innovative services.
%20(Small).png?width=480&height=637&name=micmoor57_An_Indian_female_doctor_in_her_forties_in_blue_scrubs_88a53d2b-bcf0-47e9-8dba-e9f8e3c7c63e%20(1)%20(Small).png)
ADDRESSING THE CHALLENGE
The Modern PA Process is Broken
Outdated PA systems, fragmented tech, and manual processes not only contribute to an estimated $950B in administrative costs but also cause 94% delays in patient treatment. As prior authorization demands grow, healthcare organizations struggle to balance immediate and long-term goals with delivering optimal patient care. Existing automation capabilities meet business needs, but do not deliver high impact value.
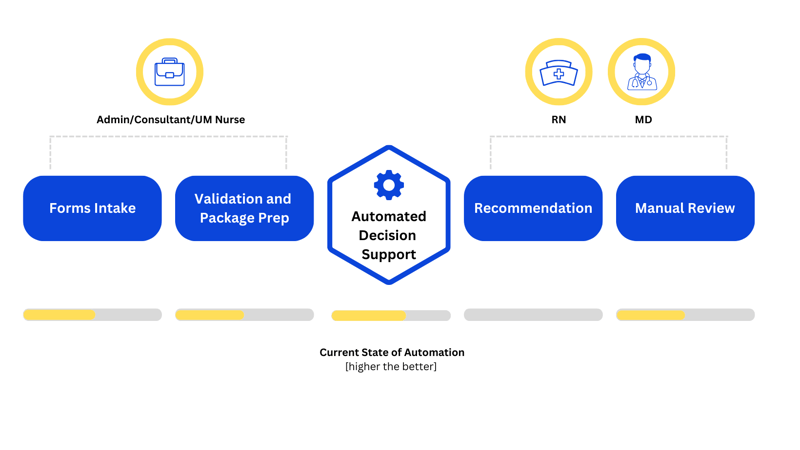
Modular AI-Enabled Services
NexAuth offers four distinct AI-enabled services. Each service is crafted with flexibility at its core. Choose and integrate one or more services that align perfectly with your priorities.
AI-enabled document processing, standardization, storage and querying of prior auth submission data.
Intelligent algorithms search patient-specific information for more than 2,000 payers, clearinghouse databases, and direct connections infrastructure to find more active coverage for healthcare billers.
A service that ingests submission data, policy coverage, evidence-based data, medical history, and guidelines and uses Vertex AI to provide a personalized approve/deny recommendation for a specific prior authorization.
A service that processes coverage details, policy information, and evidence-based data for specific prior auth requests, utilizing Vertex AI to aid clinicians in reviewing and quickly summarizing key information and responding to their queries.
Navigate prior authorization complexities with confidence
NexAuth equips payers with intelligent automation to close the gap in PA and enable seamless continuity of care with modular AI-enabled services built on the Google Cloud Platform.

Seamlessly extend your existing systems or add further transformative functionality to a newly adopted end-to-end platform.

Select one or all of NexAuth's services, each designed to meet your specific requirements.

Achieve agility and scalability to stay ahead of the evolving healthcare landscape.
.png)
Realize the full potential of innovation without the drawbacks of complex change management.
Everything you need to know
FAQs
NexAuth is a suite of AI-enabled services for quick integration with payer-managed prior authorization workflows. It streamlines processes, cuts costs, and improves member satisfaction, while offering the flexibility to deploy one or all of its AI-enabled services to enhance automation and efficiency.
Let's Talk
Ready to experience AI-enabled prior authorization?
Break down traditional care barriers and re-imagine prior authorization automation fueled by efficiency and real-time decision-making.
FEATURED GUIDE
The ultimate guide to prior authorization
Download this guide from our partner, Myndshft, to get answers to all of your top-of-mind questions around the prior authorization process.

Insights from the P/E blog
What Google’s 2026 AI Agent Report Gets Right—and What Healthcare Leaders Still Need to Solve
-1-1.jpeg)
Two Ways to Apply AI to Claims Integrity. One Foundation for Both.